Andropause, Somatopause, and Other Age Related Hormone Changes in Men
Posted By: Steve Parcell  Posted On: January 27, 2014
Posted On: January 27, 2014
Do Men Go Through Menopause?
By Steve Parcell, ND
By the time men are between the ages of 40 and 55, they can experience a phenomenon similar to menopause, called andropause. Alternative names for Andropause have been suggested including the Male Menopause, Androgen Deficiency in Aging Male (ADAM) and Partial Androgen Deficiency in Aging Male (PADAM) . Unlike women, men do not have a clear-cut benchmark such as the end menstruation to mark this transition. Andropause is defined as a time in the life of men when hormones decline. Most of us know that testosterone declines as we age but many people do not realize that other important hormones can be affected.

Somatopause
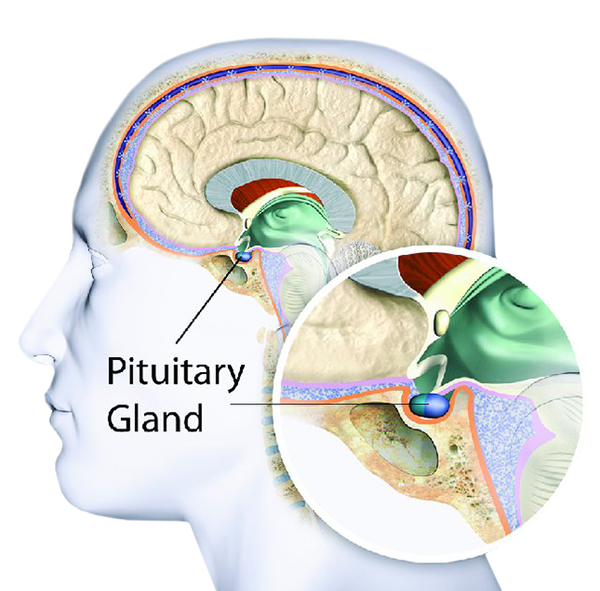
Somatopause is a decline in growth hormone levels. Somatopause signifies the gradual decline in growth hormone production by the adult pituitary gland in both men and women that begins at approximately age 30 and continues at a steady rate throughout life. Growth hormone is secreted by the anterior pituitary gland. A very busy gland, the anterior pituitary also secretes thyroid stimulating hormone (promoting thyroid activity), adrenal corticotropic hormone (promoting adrenal activity) and other hormones.
When levels of these hormones go down cognition (brain function), energy level, libido (sex drive), and body shape can change. A typical patient will complain of depression, low libido, fatigue and difficulty losing fat or difficulty gaining muscle despite many trips to the gym. Memory loss is also a common occurrence with andropause and may be due to declining hormones. Night sweats; flushes, and erectile dysfunction (ED) may also be seen.
The circulating levels of hormones that may decline in aging males are:
![]() Dehydroepiandrosterone (DHEA) and dehydroepiandrosterone sulfate (DHEAS)
Dehydroepiandrosterone (DHEA) and dehydroepiandrosterone sulfate (DHEAS)
![]() Growth hormone and insulin-like growth factor-1 (IGF-1)
Growth hormone and insulin-like growth factor-1 (IGF-1)
![]() Other hormones including thyroid
Other hormones including thyroid
Total Testosterone declines about 100 ng/dL per decade after age 50, but “free bioavailable” testosterone decline far more dramatically. Bioavailable testosterone level<70 ng/dL or total testosterone level<300 ng/dL are diagnostic of a problem called male hypogonadism . Male hypogonadism can lead to symptoms such as decreased libido, erectile dysfunction, fatigue, loss of energy, muscle weakness and even memory loss.
Why Does it Happen?
In the aging male reduction in testosterone levels is due mainly to a decline cells that make testosterone in the testicles. It can also occur because the brain is not giving the right messages to the testes. A normal decline starts in early middle age and then progresses in a linear fashion throughout life .
Mirroring this decline in testosterone concentration is an age associated increase in sex hormone binding globulin (SHBG), resulting in a decline available testosterone. The higher your SHBG levels are the more testosterone is “locked up” and not available for use. This results in increasing body fat and loss of muscle . Concentrations of testosterone decrease by as much as 50% between the ages of 25 and 75 years.
Getting Tested
There are urine, saliva, and blood tests available. I recommend a blood test to check free and total testosterone, IGF1 (growth hormone or HGH), estrogen, DHEA, and thyroid hormones. Other routine labs will can be conducted to further rule out other causes.

Hypogonadism (diagnosis of below normal testosterone) is a pathological state which is associated with several other factors that increase the risk of cardiovascular disease (obesity, higher waist:hip ratio; higher concentrations of glucose (blood sugar), insulin, total cholesterol, low density lipoprotein cholesterol (LDL), triglycerides, etc.). These levels of risk factors can be improved by testosterone administration . Testosterone replacement therapy in men with hypogonadism improves muscle mass, muscle bulk, and strength . One should never undergo testosterone therapy without a consultation and approval of a physician.

Low growth hormone levels may also be found. This is called “adult growth hormone deficiency” or “somatopause” and treatment options include Trans –D Tropin, HGH injections or secretogogues. Trans-D Tropin encourages your body to make its own HGH naturally whereas HGH injections are actual human growth hormone and can be quite expensive. There is also more potential for adverse effects.

Pioneering studies carried out by Rudman et al. showed that GH administration to elderly subjects with low growth hormone levels resulted in reversal of many of the changes associated with GH deficiency, namely an increase in lean body mass and bone mineral density and a reduction in body fat and plasma cholesterol. Other researchers showed positive effects of GH on muscle mass, central fat, cholesterol and exercise capacity. In many instances there was a positive interaction between GH and testosterone, but it appeared that GH showed the most potent anabolic effects . Presently, however, more studies are needed to prove the absolute safety of HGH injections.